Frostbite is an injury caused by the freezing of skin and underlying tissues, causing the skin to become cold, red, numb, hard, and pale. It most commonly affects exposed skin on the fingers, toes, nose, ears, cheeks, and chin, but can also occur on skin that is covered by gloves or clothing.
The first stage of frostbite, known as frostnip, usually does not cause permanent skin damage and can be treated with first-aid measures, such as re-warming the skin. However, all other stages of frostbite require medical attention as they can cause damage to skin, tissues, muscles, and bones. Complications of severe frostbite can include infection and nerve damage.
Signs and symptoms of frostbite include:
****At first, cold skin and a tingling or burning sensation
****Skin numbness
****Changes in skin color, such as red, white, bluish-white, or grayish-yellow
****Hard or waxy-looking skin
****Clumsiness due to joint and muscle stiffness
****Blistering after re-warming in severe cases.
Frostbite is most common on the fingers, toes, nose, ears, cheeks, and chin. However, due to skin numbness, you may not realize you have frostbite until someone else points it out.
Frostbite occurs in several stages:
Frostnip: The first stage of frostbite is frostnip. With this mild form of frostbite, your skin may pale or turn red and feel very cold. Continued exposure leads to prickling and numbness in the affected area. As your skin warms, you may feel pain and tingling. Frostnip doesn't cause permanent damage to the skin.
Superficial Frostbite: The second stage of frostbite results in reddened skin that turns white or pale. The skin may remain soft, but ice crystals may form in the tissues. Your skin may start to feel warm, which is a sign of serious skin involvement. If you treat frostbite at this stage with re-warming, the surface of your skin may appear mottled, blue, or purple, and you may experience stinging, burning, and swelling. A fluid-filled blister may develop 24 to 36 hours after rewarming the skin.
Severe (Deep) Frostbite: As frostbite progresses, it affects all layers of the skin and underlying tissues. You may feel numb, lose all sensation of cold, experience pain or discomfort in the affected area, and joints or muscles may stop working. Large blisters may form 24 to 48 hours after rewarming, and after that, the area may turn black and hard as the tissue dies.
Causes: Frostbite occurs when the skin and underlying tissues freeze. The most common cause of frostbite is exposure to cold-weather conditions. But it can also be caused by direct contact with ice, freezing metals or very cold liquids.
Specific conditions that lead to frostbite include: wearing clothing that isn't suitable for the conditions, staying out in the cold and wind for extended periods, particularly when the air temperature is below 5°F (-15°C) and wind chill is -16.6°F (-27°C) or lower, and touching extremely cold materials like ice, cold packs, or frozen metal.
Risk factors
The following factors increase the risk of frostbite:
Medical conditions that affect your ability to feel or respond to cold, such as dehydration, exhaustion, diabetes, or poor blood flow in your limbs.
****Alcohol or drug use.
****Smoking.
****Fear, panic, or mental illness that can inhibit good judgment or hamper your ability to respond to cold.
****A history of frostbite or cold injury.
****Being an infant or an older adult, both of whom may have difficulty producing and retaining body heat.
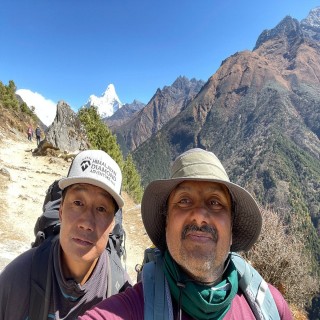
****Being at high altitude, which reduces the oxygen supply to the skin.
Prevention:
Here are some tips to help you stay safe and warm:
****Wear a hat, mittens and insulated, waterproof boots.
****Cover your mouth with a scarf to protect your lungs.
****Keep yourself dry and change wet clothes immediately.
****Heavy woolen or windproof materials make the best headwear to protect from cold.
****Take frequent breaks in warm, dry shelters.
****Keep moving to improve circulation, especially your hands and feet.
****Stay hydrated and eat well-balanced meals.
****Avoid alcohol and smoking, as these can increase your risk of frostbite.
****Wear socks and sock liners that fit well, wick moisture and provide insulation.
****You might also try hand and foot warmers. Be sure the foot warmers don't make your boots too tight, restricting blood flow.
Air trapped between the layers of clothing acts as insulation against the cold. Wear windproof and waterproof outer garments to protect against wind, snow, and rain. Choose undergarments that wick moisture away from your skin. Change out of wet clothing — particularly gloves, hats, and socks as soon as possible.
Mittens provide better protection. Or try a thin pair of glove liners made of a wicking material (like polypropylene) under a pair of heavier gloves or mittens
Watch for signs of frostbite:
****Early signs of frostbite include red or pale skin, prickling, and numbness.
Plan to protect yourself:
****When traveling in cold weather, carry emergency supplies and warm clothing in case you become stuck. If you'll be in remote territory, tell others your route and expected return date.
****Don't drink alcohol if you plan to be outdoors in cold weather.
****Alcoholic beverages cause your body to lose heat faster.
****Eat well-balanced meals and stay hydrated.
****Doing this even before you go out in the cold will help you stay warm. And if you do become cold, drinking warm, sweet beverages, such as hot chocolate, will help you warm up.
****Keep moving.
****Exercise can get the blood flowing and help you stay warm, but don't do it to the point of exhaustion.
Treatments and drugs:
Treatment for frostbite includes first-aid, care and medical treatment, depending on the severity of the frostbite. You can treat very mild frostbite (frostnip) with first-aid measures. All other frostbite requires medical attention.
First-aid care:
****Check for hypothermia.
****Get emergency medical help if you suspect hypothermia.
Protect your skin from further exposure:
If you're outside and your hands are frostbitten, warm them by tucking them into your armpits. To protect your face, nose, and ears, cover them with dry, insulated gloves or a scarf. Avoid rubbing the affected areas and never apply snow directly to frostbitten skin, as it can cause further damage.
Get out of the cold:
Once you're indoors, remove wet clothes. Wear cold protective clothes
Gently re-warm frostbitten areas:
****Deepen your hands or feet in the warm water of 99 to 108 F (37 to 42* C) for 15 to 30 minutes. If a thermometer isn't available, test the water by placing an uninjured hand or elbow in it. It should feel very warm, not hot.
****Don't re-warm frostbitten skin with direct heat, such as a stove, heat lamp, fireplace or heating pad. These can cause burns.
****Don't soften the affected areas if it will freeze again
****If your frostbitten hands have thawed, wrap them up securely to prevent them from re-freezing.
Take pain medicine:
If you are in pain, take over-the-counter ibuprofen (Advil, Motrin IB, others) to reduce pain and inflammation.
Don't walk on frostbitten feet or toes if possible:
This further damages the tissues.
Know what to expect as skin thaws:
If the skin turns red and you feel tingling and burning as it warms, normal blood flow is returning. But seek emergency medical attention if the numbness or pain remains during warming or if blisters develop.
Medical treatment:
Re-warming the skin:
If it hasn't been done already, your doctor will re-warm the area using a warm-water bath for 15 to 30 minutes. The skin may turn soft and look red or purple. You may be encouraged to gently move the affected area as it re-warms.
Oral pain medicine
Because the re-warming process can be painful, your doctor is likely to give you a drug to ease the pain.
Protecting the injury:
Once your skin thaws, your doctor may loosely wrap the area with sterile sheets, towels or dressings to protect the skin. You may need a brace or splint if the bone or muscle is involved. And you may need to elevate the affected area to reduce swelling.
Removal of damaged tissue (debridement):
To heal properly, frostbitten skin needs to be free of damaged, dead or infected tissue. To better distinguish between healthy and dead tissue, your doctor may wait for one to three months before removing damaged tissue.
Whirlpool therapy:
Soaking in a whirlpool bath (hydrotherapy) can aid healing by keeping skin clean and naturally removing dead tissue. You'll be encouraged to move gently the affected area while it is underwater.
Infection-fighting drugs:
If your skin or blisters appear infected, your doctor may prescribe oral antibiotics.
Clot-busting drugs:
You may receive an intravenous injection (IV) of a drug that helps restore blood flow (thrombolytic), such as tissue plasminogen activator (TPA). Studies of people with severe frostbite show that TPA lowers the risk of amputation. But these drugs can cause serious bleeding and are typically used only in the most serious situations and within 24 hours of exposure.
Wound therapy:
If you have a complex wound, your doctor might suggest a technique called vacuum-assisted closure therapy to promote healing.
Surgery:
In severe cases, surgery or amputation may be necessary to remove the dead or decaying tissue.
Hyperbaric oxygen therapy:
Hyperbaric oxygen therapy involves breathing pure oxygen in a pressurized room. Some patients showed improved symptoms after this therapy. But more study is needed.